Aflatoxin is a secondary metabolite produced by toxigenic strains of A.
flavus and A. parasiticus. Chemically, aflatoxins belong to the
bifuranocoumarin group, with aflatoxins B1 (AFB1), B2 (AFB2), G1 (AFG1)
and G2 (AFG2) being the most toxic. Liver is the main organ affected by
these toxins.
Aflatoxin is a secondary metabolite produced by toxigenic strains of A.
flavus and A. parasiticus. Chemically, aflatoxins belong to the
bifuranocoumarin group, with aflatoxins B1 (AFB1), B2 (AFB2), G1 (AFG1)
and G2 (AFG2) being the most toxic. Liver is the main organ affected by
these toxins.Aflatoxin is a type of mold that is considered a human carcinogen. It’s found in certain commonly eaten foods including peanuts, peanut butter and corn, and is most harmful in parts of the world where people consume large amount of these foods, such as Asia and Africa. The species of molds that combine to form aflatoxin grow in soils when conditions are just right, including when decaying food, plants, hay and grains are piled together to decompose in areas with high moisture and high temperatures.
There are actually at least 13 different types of naturally-occurring aflatoxin toxic molds that researchers have been able to identify. Of the 13 species, the type called aflatoxin B1 is considered the most toxic, capable of causing health problems such as liver disease or cancer, autoimmune responses, digestive issues and in rare cases even death. Research has shown that consuming aflatoxin through the food supply is one of the major causes of liver disease (specifically the type called hepatocellular carcinoma) in certain countries such as China and Africa.
Poultry is considered as the most susceptible animal species to aflatoxins. A meta-analysis (Andretta et al 2011) carried out on broiler performance in response to mycotoxins showed that aflatoxin (average concentration 0.95mg/kg of feed) and ochratoxin had the biggest effects on broiler performance. Aflatoxins on average significantly reduced feed intake by 10% and growth rate by 12%. Aflatoxins also significantly increased liver weight by 22% and the weight of kidneys, lungs, gizzard and the heart. Aflatoxins presented the most important effects of all mycotoxins on organ weight in broilers.
What Does Aflatoxin Do and Where Does It Come From?
 Chemically speaking, aflatoxin is a type of “mycotoxin” which is produced by two different species of mold: Aspergillus flavus and Aspergillus parasiticus.
There are natural molds found around the world and concentrated most in
the human food supply in areas with wet and warm climates. It’s also
possible for aflatoxin mold to form in grains grown under poor
conditions, such as those experiencing droughts.
Chemically speaking, aflatoxin is a type of “mycotoxin” which is produced by two different species of mold: Aspergillus flavus and Aspergillus parasiticus.
There are natural molds found around the world and concentrated most in
the human food supply in areas with wet and warm climates. It’s also
possible for aflatoxin mold to form in grains grown under poor
conditions, such as those experiencing droughts.The strains of aflatoxin most common in foods include B1, B2, G1 and G2. After humans or other mammals consume aflatoxin metabolic processes turn then into metabolites M1 and M2 which have ” high carcinogenic potential.” International Agency for Research on Cancer has classified aflatoxin B1 as a “Group I carcinogen” that’s capable of raising the risk for cancer. Aflatoxin seems to affect the ways that cells reproduce and also targets the liver, affecting the way that other substances are metabolized and eliminated, and possibly increasing food allergy reactions.
There are many different types of molds and fungus that can grow in food, including various species of mycotoxins, but aflatoxin has gained attention more than most others because studies have found clear evidence of its potential for causing carcinogenic effects. In animal studies, high levels of aflatoxin consumption has been shown to be poisonous, and in human observation studies aflatoxin consumption correlates with an increased the risk for certain illnesses and dangerous symptoms.
Over the last 100 years, there are have also been several occurrences when large populations of livestock (cattle, ducks, chicken, etc.) have died due to contamination of their food supply, especially peanut flour or cottonseed, which can sometimes become home to a dozen different strains of aflatoxin
Unfortunately, aflatoxin makes its way into some popular “healthy” foods that aren’t actually healthy. The level of aflatoxin contamination in any given food will vary with geographic location, along with how the food was grown. Additionally, once crops are picked it matters how they are handled, processed and stored, since all of these can affect whether or not aflatoxin is able to survive and thrive. Some research shows that crops being grown in humid locations such as Brazil and China are most likely to contain aflatoxin.
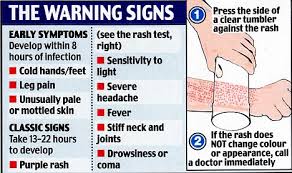
Aflatoxin Symptoms & Health Risks
People
living in Third World countries are most likely to be impacted by the
negative effects of aflatoxin poisoning, but this doesn’t mean that
developed nations are totally safe. The consumption of “staple crops”
that can contain aflatoxin, such as corn and peanuts, are used globally,
and even a small of aflatoxin in the food supply can wind up spreading
and causing problems. How badly a person is affected by aflatoxin will
depend on factors like their current state of health, level and duration
of exposure, strength of their immune and digestive system, and overall quality of their diet.
There
are two ways that aflatoxin contamination usually occurs: Either
someone consumes large amounts at once and experiences “poisoning”, or
they slowly acquire aflatoxin over time in smaller quantities. According
to the FDA, poisoning is relatively rare but more dangerous and can
lead to problems like liver cancer, mental impairments, digestive
reactions, coma, hemorrhages and malabsorption.Long-term, some of the symptoms that aflatoxin exposure can cause include:
- food allergies
- autoimmune disease reactions
- inflammation that affects the heart
- damage to the digestive organs including the liver and kidneys
- possibly a higher risk for liver cancer, viral hepatitis (HBV) or parasite infestation
- growth and development impairment
- the biggest threat is the symptoms seen in patients in liver diseases: vomiting, abdominal pain, water retention, pulmonary edema, convulsions, coma, and even death
- Research shows that aflatoxin targets the digestive organs most,
especially the liver by raising the risk for liver cancer, heptitis and
liver disease. Long-term exposure to aflatoxin
is a major risk factor for cancer of liver called hepatocellular
carcinoma, which causes liver scarring, loss of nutrients, inflammation
of the digestive tract and other serious problems that can lead to
death.
How to Avoid Aflatoxin Foods & Lower Exposure
The foods and crops most likely to be contaminated with aflatoxin include: - peanuts
- corn
- milk and cheese (rarely, meat can also become contaminated due to the spreading in aflatoxin in livestock feed)
- nuts (especially almonds, Brazil nuts, pecans, pistachios and walnuts)
- grains including quinoa
- soybeans
- figs
- dried spices
- although it’s not commonly eaten, cottonseed is also a major crop that tends to grow aflatoxin
Aflatoxin in peanuts are another major concern for the same reasons. Peanuts are consumed in high amounts in countries across Asia and also in the U.S, plus they are used in many other types of processed foods (peanut butter, cereals, packaged snacks like cookies, ice cream, etc).
Tips & Supplements that Can Help Lower Aflatoxin
Wondering what else you can do to avoid aflatoxin symptoms? Here are several tips for purchasing and handling foods, plus supplements that can boost detox effects:- Don’t keep grains and nuts (corn, peanuts, almonds, for example) for long periods of time. Try consuming them ideally within 1–2 months
- Buy the freshest ingredients you can, ideally those grown close to your location and not shipped overseas. Reputable, small sellers who grow organic crops are most likely to harvest them at the right time and keep them stored properly
- Store grains, corn and nuts in places that are dry and cool to prevent mold growth. You can even freeze them to prolong freshness
- Soak, sprout and ferment grains, beans, legumes nuts and seeds before eating them! This is an easy step you can do at home that doesn’t take much time, boosts the availability of nutrients and helps lower presence of “antinutrients” and mold
- There’s also some evidence that eating detoxifying vegetables like carrots and celery reduces the carcinogenic effects of aflatoxins and helps cleanse the liver
Consume the supplements below that can boost detoxification effects, cleanse the liver and improve digestion:
- Studies show that chlorophyllin and chlorophyll supplements help to reduce the bioavailability of aflatoxin (11)
- Milk thistle, marshmallow root and dandelion root all help cleanse the liver and can lower digestive symptoms
- Activated charcoal can help bind to aflatoxin mold and carry it out of the body more easily